- Introduction: A Healthcare Powerhouse with Hidden Inefficiencies
- Key Challenges: Why Energy Efficiency Efforts Were Falling Short
- Why Current Efforts Fall Short: The Missing Links
- A Transformative Partnership: Consulting + ESCO Expertise
- Results: A Blueprint for Sustainable and Profitable Operations
- Why This Matters to Private Healthcare Owners Everywhere
- Conclusion: A Roadmap for Continuous Improvement
- Are You Ready to Transform Your Healthcare Facilities?
- Have questions or need more clarification?
Introduction: A Healthcare Powerhouse with Hidden Inefficiencies
Private hospitals are among the most energy-intensive facilities worldwide. They operate around the clock; their critical systems (e.g., HVAC, boilers, chillers, medical gas networks) demand uninterrupted power, and advanced medical equipment often runs at full capacity. For a prominent health group with 12 private hospitals across the country, business is at an all-time high, fueled by:
- Rising demand for high-quality care.
- Strategic expansion into underserved regions.
- Investments in cutting-edge technology to improve patient outcomes.
But behind the scenes, operational inefficiencies and ageing infrastructure in the existing hospitals threaten to undermine the group’s sustainability goals and bottom line. While some hospitals boast newer devices, others struggle with aging chillers, frequent HVAC breakdowns, and outdated lighting systems—all compounded by decentralized budgeting and lack of centralized data tracking.
As they embark on sustainability reporting (Scope 1 & 2—and soon Scope 3 emissions), hospital managers realize they need a more cohesive, data-driven strategy to ensure compliance with regulations like the Energy Efficiency and Conservation Act (EECA), reduce carbon footprint, and control spiraling energy costs.
Disclaimer: This case study is a hypothetical scenario based on specific conditions and challenges commonly faced by manufacturing plants. The solutions and results described are illustrative and may vary depending on individual circumstances.
Key Challenges: Why Energy Efficiency Efforts Were Falling Short
- Aging Assets and Frequent Breakdowns
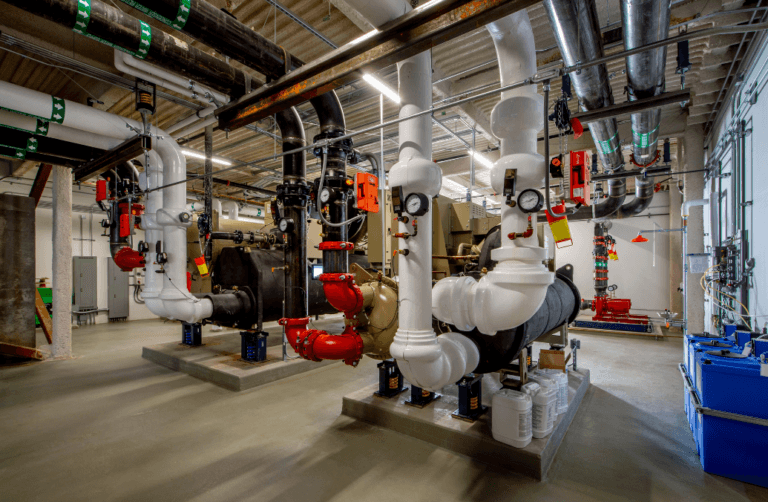
Many of the group’s hospitals are over a decade old, and their critical systems—such as HVAC, chillers, boilers, and medical gas systems—are nearing the end of their lifecycle. Frequent breakdowns not only disrupt hospital operations but also lead to higher energy consumption and unplanned maintenance costs.
🔧 Example: A hospital in the northern region experienced repeated HVAC failures during peak summer months, leading to patient discomfort and skyrocketing energy bills.
- Decentralized Budgeting and Procurement
Each hospital prepares its own budget requests for equipment upgrades and maintenance, which are then consolidated at the group level. However, the group’s financial focus is on revenue-generating activities, such as purchasing advanced medical equipment and funding new hospital developments. As a result, engineering and maintenance budgets are often cut, forcing hospitals to procure equipment independently and in a piecemeal fashion.
💰 Example: One hospital replaced its aging chiller with a high-efficiency model, while another hospital continued to operate an outdated system because its budget request was denied.
- Lack of Centralized Tracking and Data Visibility
The group has no centralized system to track energy consumption, equipment performance, or maintenance activities across its 12 hospitals. Each hospital submits manual reports, often in different formats, making it difficult to consolidate data and identify trends.
📊 Example: Solar panels installed at three hospitals are underutilized because their energy generation is not aligned with peak consumption periods. This issue goes unnoticed due to the lack of centralized monitoring.
- Compliance with EECA and Sustainability Reporting
While the hospitals have undergone energy audits and implemented some recommendations, these actions are often limited by budget constraints. The group also struggles to collect and standardize data for sustainability reporting, making it difficult to measure progress or plan future initiatives.
⚠️ Example: A hospital in the southern region struggles to meet EECA compliance due to outdated lighting systems and inefficient HVAC units.
- Interdepartmental Issues and Hierarchy Challenges
The engineering and maintenance teams are often viewed as a supporting function, with lower priority compared to departments directly involved in patient care or revenue generation. The dual reporting structure—where engineering teams report to both hospital management and the group’s central engineering department—creates confusion and delays in decision-making.
🤝 Example: The group mandates the installation of energy-efficient lighting across all hospitals, but one hospital’s engineering team argues that replacing its failing chiller should take precedence.
- Sustainability vs. Profitability
The group’s sustainability commitments often clash with its aggressive profit targets—especially amid expansions and new building developments. Upgrading to more efficient systems can be expensive up front, so sustainability initiatives get limited attention unless they promise a rapid ROI.
🌱 Example: A facility invests in high-performance windows to cut heating costs, but simultaneously postpones a critical chiller overhaul because of the steep capital expenditure.
Why Current Efforts Fall Short: The Missing Links
- Fragmented Decision-Making: Without a centralized platform, each hospital implements energy-saving measures in isolation, diluting the overall impact.
- Delayed Action: Budget constraints plus a preference for new expansions lead to postponed equipment upgrades, aggravating inefficiencies on existing campuses.
- Missed Opportunities: Efforts like solar panel installations or high-efficiency lighting can fail to deliver full benefits without real-time data analytics, usage alignment, or thorough PDCA (Plan-Do-Check-Act) cycles.
- Compliance Gaps: Outdated machinery and insufficient funding for recommended energy audits hinder full EECA compliance.
- Limited Sustainability Impact: Even well-intentioned eco-friendly measures are hamstrung by a lack of top-down coordination, funding, and consistent performance data.