Table of contents
- Introduction: A Healthcare Powerhouse with Hidden Inefficiencies
- Key Challenges: Why Energy Efficiency Efforts Were Falling Short
- Why Current Efforts Fall Short: The Missing Links
- A Transformative Partnership: Consulting + ESCO Expertise
- Results: A Blueprint for Sustainable and Profitable Operations
- Why This Matters to Private Healthcare Owners Everywhere
- Conclusion: A Roadmap for Continuous Improvement
- Are You Ready to Transform Your Healthcare Facilities?
- Next Steps
- Have questions or need more clarification?
Introduction: A Healthcare Powerhouse with Hidden Inefficiencies
Private hospitals are among the most energy-intensive facilities worldwide. They operate around the clock; their critical systems (e.g., HVAC, boilers, chillers, medical gas networks) demand uninterrupted power. Plus don’t forget, advanced medical equipment often runs at full capacity. For a prominent health group with 12 private hospitals across the country, business is at an all-time high, fueled by:
- Rising demand for high-quality care.
- Strategic expansion into underserved regions.
- Investments in cutting-edge technology to improve patient outcomes.
But behind the scenes, operational inefficiencies and ageing infrastructure in the existing hospitals threaten to undermine the group’s sustainability goals and bottom line. While some hospitals boast newer devices, others struggle with aging chillers, frequent HVAC breakdowns, and outdated lighting systems—all compounded by decentralized budgeting and lack of centralized data tracking.
As they embark on sustainability reporting (Scope 1 & 2—and soon Scope 3 emissions), hospital managers realize they need a more cohesive, data-driven strategy to ensure compliance with regulations like the Energy Efficiency and Conservation Act (EECA). This is on top of needing to reduce carbon footprint, and control spiraling energy costs.
Disclaimer: This case study is a hypothetical scenario based on specific conditions and challenges commonly faced by manufacturing plants. The solutions and results described are illustrative and may vary depending on individual circumstances.
Key Challenges: Why Energy Efficiency Efforts Were Falling Short
1. Aging Assets and Frequent Breakdowns
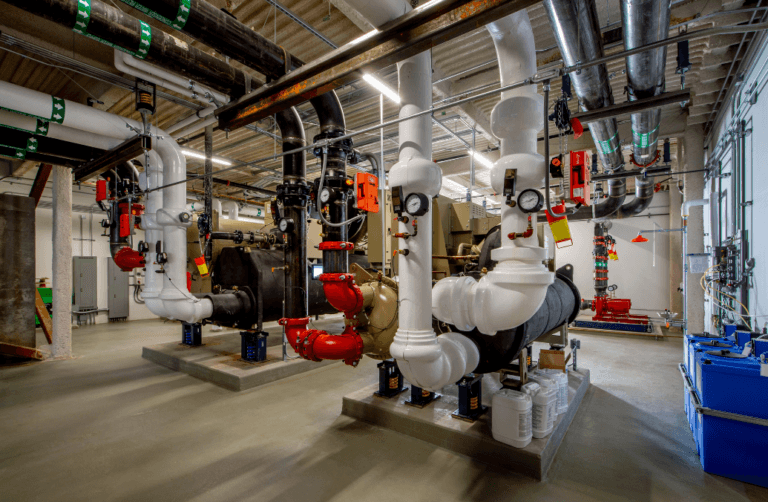
Many of the group’s hospitals are over a decade old, and their critical systems—such as HVAC, chillers, boilers, and medical gas systems—are nearing the end of their lifecycle. Frequent breakdowns not only disrupt hospital operations but also lead to higher energy consumption and unplanned maintenance costs.
🔧 Example: A hospital in the northern region experienced repeated HVAC failures during peak summer months, leading to patient discomfort and skyrocketing energy bills.
2. Decentralized Budgeting and Procurement
Each hospital prepares its own budget requests for equipment upgrades and maintenance, which are then consolidated at the group level. However, the group’s financial focus is on revenue-generating activities, such as purchasing advanced medical equipment and funding new hospital developments. As a result, engineering and maintenance budgets are often cut, forcing hospitals to procure equipment independently and in a piecemeal fashion.
💰 Example: One hospital replaced its aging chiller with a high-efficiency model, while another hospital continued to operate an outdated system because its budget request was denied.
3. Lack of Centralized Tracking and Data Visibility
The group has no centralized system to track energy consumption, equipment performance, or maintenance activities across its 12 hospitals. Each hospital submits manual reports, often in different formats, making it difficult to consolidate data and identify trends.
📊 Example: Solar panels installed at three hospitals are underutilized because their energy generation is not aligned with peak consumption periods. This issue goes unnoticed due to the lack of centralized monitoring.
4. Compliance with EECA and Sustainability Reporting
While the hospitals have undergone energy audits and implemented some recommendations, these actions are often limited by budget constraints. The group also struggles to collect and standardize data for sustainability reporting. This makes it difficult to measure progress or plan future initiatives.
⚠️ Example: A hospital in the southern region struggles to meet EECA compliance due to outdated lighting systems and inefficient HVAC units.
5. Interdepartmental Issues and Hierarchy Challenges
The engineering and maintenance teams are often viewed as a supporting function. Because of that they have lower priority compared to departments directly involved in patient care or revenue generation. The dual reporting structure—where engineering teams report to both hospital management and the group’s central engineering department—creates confusion and delays in decision-making.
🤝 Example: The group mandates the installation of energy-efficient lighting across all hospitals, but one hospital’s engineering team argues that replacing its failing chiller should take precedence.
6. Sustainability vs. Profitability
The group’s sustainability commitments often clash with its aggressive profit targets—especially amid expansions and new building developments. Upgrading to more efficient systems can be expensive up front, so sustainability initiatives get limited attention unless they promise a rapid ROI.
🌱 Example: A facility invests in high-performance windows to cut heating costs, but simultaneously postpones a critical chiller overhaul because of the steep capital expenditure.
Why Current Efforts Fall Short: The Missing Links
- Fragmented Decision-Making: Without a centralized platform, each hospital implements energy-saving measures in isolation, diluting the overall impact.
- Delayed Action: Budget constraints plus a preference for new expansions lead to postponed equipment upgrades, aggravating inefficiencies on existing campuses.
- Missed Opportunities: Efforts like solar panel installations or high-efficiency lighting can fail to deliver full benefits without real-time data analytics, usage alignment, or thorough PDCA (Plan-Do-Check-Act) cycles.
- Compliance Gaps: Outdated machinery and insufficient funding for recommended energy audits hinder full EECA compliance.
- Limited Sustainability Impact: Even well-intentioned eco-friendly measures are hamstrung by a lack of top-down coordination, funding, and consistent performance data.
A Transformative Partnership: Consulting + ESCO Expertise
Realizing that the stopgap measures, firefighting and “seasonal” improvements were insufficient, the health group partnered with a specialized consulting firm that combines Big 5 consulting methodology with Energy Service Company (ESCO) solutions. The goal: unearth hidden inefficiencies, standardize processes, and craft a forward-thinking energy management strategy aligned with compliance and sustainability targets.

Project Phases and Approach
1. Holistic Diagnostics
The consulting team performed site audits and stakeholder interviews with hospital management, engineering teams, and finance leaders. They collated historical energy bills, equipment performance data, and prior energy audit reports.
Key Insight: Different hospitals had similar issues—outdated lighting, suboptimal HVAC usage, inconsistent procurement—but lacked a unified approach to fix them.
2. Data Consolidation & Visualization
The team inventoried all major systems—HVAC, chillers, boilers, (and in some cases, considered upgrading from boilers to heat pumps), lighting nodes, and medical gas—creating a centralized data repository. This was then connected to an energy analytics platform providing real-time dashboards for each hospital.
- PDCA Enabled: With real-time data, management can Plan new upgrades, Do pilot initiatives, Check through analytics, and Act on insights to refine strategies.
3. Priority-Based Budgeting
Using aggregated data, the consulting team helped prioritize upgrades and maintenance tasks based on:
- Energy ROI (e.g., large chillers or HVAC systems with high consumption).
- Compliance Impact (for the EECA audits).
- Patient Comfort (e.g., consistent climate control for patient safety).
- Synergies (i.e., group-purchasing for discounts on large equipment orders).
- Potential for Boiler-to-Heat-Pump Conversions: Due to significant energy-saving potential and reduced carbon emissions, the health group began evaluating heat pumps as a cost-effective way to replace aging boilers, especially for sites with near-future boiler replacement needs.
4. Standardizing Procurement and Maintenance Protocols
By implementing a centralized procurement framework, each hospital now benefits from bulk-buy discounts and standardized quality assessments. This also strengthens post-purchase servicing contracts.
- Simplified vendor management reduces the administrative load on individual hospital teams.
- Energy Performance Contracting (EPC): The group explored EPC options to finance significant equipment overhauls—like chillers, HVAC systems, and boiler-to-heat-pump conversions—reducing initial capital outlay. Under EPC, the ESCO guarantees energy savings, and repayments are made from the cost savings realized, thus mitigating financial risk.
5. Energy Monitoring System (EMS) Integration
❤️ Marketing Spotlight: One critical piece of this transformation involved integrating an EMS like Innovast’s “InnoSense” energy and asset management solution. InnoSense supports:
- Real-Time Monitoring of energy usage at each hospital, detecting anomalies instantly.
- Predictive Maintenance alerts to reduce downtime and extend asset life.
- Comprehensive Reporting for compliance and sustainability tracking—Scope 1, 2, and soon 3.
- Adaptive Planning: The system helps plan future expansions or upgrades by simulating ROI scenarios.
6. Change Management & Culture Shift
The consulting team facilitated executive workshops and training sessions to reposition engineering and maintenance teams as strategic partners rather than cost centers. This shift not only improved morale but also accelerated decision-making for infrastructure improvements.
Granular Data for Cost Allocation: With the new analytics platform, hospitals gained unprecedented detail on cost per patient and cost per treatment in various departments— tying energy usage directly to operational and revenue metrics.
Marketing & Analytics Impact: Such granular data enabled the hospital’s marketing and analytics teams to devise more targeted service packages, identify high-return or underutilized service lines, and optimize patient programs (e.g., specialized cardiac care, premium orthopedic services, or elective surgery bundles). This directly contributed to higher profit margins and more efficient budget allocations.
Results: A Blueprint for Sustainable and Profitable Operations
1. Substantial Energy Cost Reductions
- 15% lower energy consumption in the first year across the entire hospital network.
- Large hospitals with advanced upgrades have already seen up to 25% in energy savings.
- Predicted ROI within 2.5 years due to real-time data insights enabling proactive interventions.
- Notable Spotlight: Early studies project even greater savings once boiler-to-heat-pump conversions are finalized for sites with older boiler systems.
2. Centralized Visibility & Decision-Making
- Unified Dashboards: Every site’s energy consumption, equipment status, and maintenance logs are accessible from a single platform.
- Improved PDCA: Hospital administrators now refine their energy strategies in iterative cycles, ensuring continuous improvement based on live data.
- Detailed Costing: The system’s granularity means leadership can accurately calculate cost per patient and per treatment, unlocking deeper financial insights.
3. Reduced Unplanned Downtime
- Breakdowns dropped by up to 30% for critical systems like HVAC and boiler units.
- Predictive maintenance extends equipment lifespan, saving on replacement costs and preventing sudden failures during peak patient loads.
4. Streamlined Compliance & Sustainability Reporting
- EECA compliance improved through consistent auditing and quicker follow-ups, ensuring a safer, greener operation.
- The group successfully reports Scope 1 & 2 emissions, with a streamlined path to Scope 3 confirmations—confidence-building for external stakeholders and investors.
- Financing Upgrades via EPC: By leveraging Energy Performance Contracting, the group offsets upfront capital costs with guaranteed energy savings, accelerating large-scale improvements without straining budgets.
5. Cultural Integration of Sustainability and Profitability
- A culture shift positions sustainability projects not as “add-on costs” but as measurable business improvements with proven ROI and brand benefits.
- Solar panel utilization jumped by 25%, thanks to usage realignment based on analytics.
- Marketing & Profitability: With clarity around operational costs, the marketing team launched higher-margin patient programs (e.g., “Executive Health Packages,” “Robotics-Assisted Surgery Bundles”), applying precise cost modeling to optimize pricing and service offerings.
Why This Matters to Private Healthcare Owners Everywhere
Private healthcare facility owners worldwide often underestimate the complexity of managing ageing infrastructures, ensuring compliance, and maintaining profit margins. While many do the “best they can” with manual logs, sporadic audits, and ad-hoc upgrades, true transformation demands:
- Centralized Data & Visibility: Real-time dashboards to identify issues and measure ROI for each hospital.
- Strategic Budgeting & Procurement: Coordinated spending on high-impact upgrades ensures maximum energy savings and cost benefits.
- Stakeholder Alignment: Engaging engineering teams, hospital admin, and central leadership in a single, transparent process fosters synergy.
- Sustainability as a Business Driver: Energy-efficient measures and greener operations can create measurable ROI while enhancing the institution’s public image.
- Innovative Financing Approaches: Leveraging Energy Performance Contracting can unlock upgrades that might otherwise be shelved due to capital constraints.
By integrating technology solutions, replacing outdated boilers with efficient heat pumps, and following a data-driven PDCA cycle, private healthcare providers can realize immediate energy savings while building a solid foundation for long-term sustainability. Moreover, the granular cost analysis that emerges from such centralized systems can uncover new revenue streams and marketing opportunities to improve overall profitability.
Conclusion: A Roadmap for Continuous Improvement
This case study highlights the journey of a 12-hospital health group from fragmented energy management to a cohesive, data-driven model of sustainability. Through real-time analytics, predictive maintenance, and strategic prioritization, the group not only lowered its energy footprint but also positioned itself favorably for future expansions and regulatory changes.
- Immediate Impact: Lower operating costs, boosted patient comfort, and enhanced regulatory compliance.
- Long-Term Benefits: Inspired confidence among stakeholders, streamlined sustainability reporting, and developed a blueprint for growth without compromising eco-responsibility or profitability.
- Additional Gains: From boiler-to-heat-pump conversions and EPC financing to granular cost modeling and refined marketing strategies, the group consistently finds new levers for growth and profitability.
Are You Ready to Transform Your Healthcare Facilities?
If you’re a private healthcare owner, administrator, or manager grappling with similar challenges—ageing infrastructure, high operational costs, or tighter sustainability mandates—understand that success lies in harnessing the power of real-time data and expert guidance. By embracing centralized asset tracking, advanced analytics, and a unified approach, you can scale your impact exponentially and future-proof your healthcare operations.
Next Steps
- Evaluate your available actionable data, existing equipment, usage patterns, and compliance gaps.
- Engage a cross-functional task force (management, engineering, finance) to unify goals.
- Explore bundling major upgrades to leverage volume discounts.
- Implement a PDCA cycle backed by data analytics for ongoing improvements.
- Consider specialized partners (Like Us!) who can tailor the perfect synergy between technology, sustainability, and financial ROI—favoring innovative strategies like heat pump adoption and Energy Performance Contracting to fund meaningful changes.
Start your journey toward a more profitable, sustainable future in healthcare today! If you have any further questions or would like specific guidance, feel free to ask—together, we can design a robust plan for ongoing success.
Have questions or need more clarification?
Let me know if you’d like additional details on procurement strategies, predictive maintenance programs, or how to integrate boiler-to-heat-pump conversions and EPC financing into your current setup. We are here to help you navigate the complex world of energy-efficient healthcare operations and ensure your hospitals meet both financial and environmental objectives.
Visit www.innovast.asia to learn more and begin your journey toward operational excellence and sustainable healthcare.